|





|
Vitamin D Can Prevent Cancer
According to
researchers at the Moores Cancer Center at the University of
California, San Diego (UCSD) increased levels of Vitamin D3 could
prevent 600,00 cases of breast and colorectal cancers each year.
150,000 in the US alone. This applies especially to countries north
of the equator.
Low levels of Vitamin D also contribute to many other human health
conditions. It is a necessary Vitamin.
"A wealth of evidence suggests that rickets is the tip of a Vitamin
D insufficiency/deficiency iceberg. A lack of Vitamin D can also
trigger infections (influenza and tuberculosis), autoimmune diseases
(multiple sclerosis, Type 1 diabetes, rheumatoid arthritis, and
inflammatory bowel disease), cardiovascular disease, and cancer.
Practitioners of conventional medicine (i.e., most MDs) are just
beginning to appreciate the true impact of Vitamin D deficiency. In
1990, medical journals published less than 20 reviews and editorials
on Vitamin D. Last year they published more than 300 reviews and
editorials on this Vitamin/hormone. This year, on July 19, 2007,
even the New England Journal of Medicine, the bellwether of
pharmaceutically-oriented conventional medicine in the U.S.,
published a review on Vitamin D that addresses its role in
autoimmune diseases, infections, cardiovascular disease, and cancer
(New England Medical Journal 2007;357:266–281)." - Donald Miller, cardiac
surgeon and Professor of Surgery at the University of Washington in
Seattle.
The human body can create Vitamin D through exposure to sunlight. In
fact it sounds like lack of Vitamin D is worse than any excess exposure
to the sun.
Vitamin D in a New Light
by Donald W. Miller, Jr., MD
There are thirteen Vitamins humans need for growth and development
and to maintain good health. The human body cannot make these
essential bio-molecules. They must be supplied in the diet or by
bacteria in the intestine, except for Vitamin D. Skin makes
Vitamin D when exposed to ultraviolet B (UVB) radiation from the
sun. A light-skinned person will synthesize 20,000 IU (international
units) of Vitamin D in 20 minutes sunbathing on a Caribbean beach.
A growing body of evidence indicates that that Vitamin D can prevent
a whole host of cancers – colon, breast, lung, pancreatic, ovarian,
and prostate cancer among them. Colon cancer rates are 4 to 6 times
higher in North America and Europe, where solar radiation is less
intense, particularly during the winter months, compared to the
incidence of colon cancer near the equator. People with low blood
levels of Vitamin D and those who live at higher latitudes are at
increased risk for acquiring various kinds of cancer. Many
epidemiological, cohort, and case control studies prove, at least on
a more likely than not basis, that Vitamin D supplements and
adequate exposure to sunlight play an important role in cancer
prevention (Am J Public Health 2006;96:252–261).
A Creighton University study has shown that women over the age of 55
who took a 1,100 IU/day Vitamin D supplement, with calcium, and were
followed for 4 years had a highly statistically significant (P
<0.005) 75% reduction in breast cancer (diagnosed after the first 12
months) compared with women who took a placebo (Am J Clin Nutr
2007;85:1568–1591).
New research suggests that influenza is also a disease triggered by
Vitamin D deficiency. Influenza virus exists in the population
year-round, but influenza epidemics are seasonal and occur only in
the winter (in northern latitudes), when Vitamin D blood levels are
at their lowest.
Our species evolved in equatorial Africa where the sun, shining
directly overhead, supplies its inhabitants with year-round
ultraviolet B photons for making Vitamin D. Our African ancestors
absorbed much higher doses of Vitamin D living exposed in that
environment compared to the amount most humans obtain today. A
single mutation that occurred around 50,000 years ago is responsible
for the appearance of white skin in humans. It turns out that a
difference in one rung, or base pair, in the 3 billion-rung DNA
ladder that constitutes the human genome determines the color of
one’s skin (Science 2005;310:1782–1786). White skin, with less
melanin, synthesizes Vitamin D in sunlight six times faster than
dark skin. People possessing this mutation were able to migrate to
higher latitudes, populate Europe, Asia, and North America, and be
able to make enough Vitamin D to survive.
The majority of the world’s population now lives above latitude 35°
N and is unable to synthesize Vitamin D from sunlight for a period
of time in winter owing to the angle of the sun. At a large solar
zenith angle, ozone in the upper atmosphere will completely block UVB radiation. In Seattle (47° N) and London (52° N), from October
to April UVB photons are blocked by the atmosphere so one’s skin
cannot make Vitamin D. (The half-life of circulating Vitamin D is
approximately one month.) Making matters worse, even when UVB
radiation is available in sunlight, health authorities, led by the
American Academy of Dermatology, warn people to shield themselves
from the sun to avoid getting skin cancer.
Except for oily fish like (wild-only) salmon, mackerel, and sardines
and cod liver oil – and also sun-dried mushrooms – very little
Vitamin D is naturally present in our food. Milk, orange juice,
butter, and breakfast cereal are fortified with Vitamin D, but with
only 100 IU per serving. A person would have to drink 200 8-oz.
glasses of milk to obtain as much Vitamin D as skin makes fully
exposed to the noonday sun.
The U.S. Food and Nutrition Board in the Institute of Medicine puts
the Recommended Dietary Allowance (RDA) for Vitamin D at 200 IU for
children and adults less than 50 years old, 400 IU for adults age
50–70, and 800 IU for adults over the age of 70. Most multivitamin
preparations contain 400 IU of Vitamin D. These guidelines are
directed towards maintaining bone health and are sufficient to
prevent rickets – but not cancer, cardiovascular disease, multiple
sclerosis, or influenza. Without evidence to support it, the board
arbitrarily set the safe upper limit for Vitamin D consumption at
2,000 IU/day.
A majority of Americans have insufficient or deficient Vitamin D
blood levels. In veterans undergoing heart surgery at the Seattle VA
hospital, I found that 78% had a low Vitamin D level: 12% were
insufficient; 56%, deficient; and 10% were severely deficient.
There are two kinds of Vitamin D supplements: Vitamin D3 (cholecalciferol),
the kind our skin makes, and Vitamin D2 (ergocalciferol), a
synthetic variant made by irradiating plants. Vitamin D2 is
only 10–30% as effective in raising 25-hydroxyVitamin D blood levels
compared to Vitamin D3, leading the authors of a recent study
conclude, "Vitamin D2 should not be regarded as a nutrient suitable
for supplementation or fortification" (Am J Clin Nutr
2006;84:694–697).
Concerns about Vitamin D toxicity are overblown, along with those
about sun exposure. As one researcher in the field puts it,
"Worrying about Vitamin D toxicity is like worrying about drowning
when you’re dying of thirst." A person must consume 50,000 IU a day
for several months before hypercalcemia (an elevated calcium level
in the blood, which is the initial manifestation of Vitamin D
toxicity) might occur. Vitamin D in a physiologic dose (5,000 IU/day)
prevents the build up of calcium in blood vessels. (Circulation
1997;96:1755–1760). If one takes 10,000 IU of Vitamin D a day and
spends a lot of time in the sun, it would be prudent to check
Vitamin D blood level to ensure that it does not exceed 100 ng/ml.
Sensible sun exposure should be encouraged, not maligned. If one
avoids sunburn, the sun’s health-giving benefits far outweigh its
detrimental effects. A large body of evidence indicates that
sunlight does not cause the most lethal form of skin cancer,
malignant melanoma. A U.S. Navy study found that melanoma occurred
more frequently in sailors who worked indoors all the time. Those
who worked outdoors had the lowest incidence of melanoma. Also, most
melanomas appear on parts of the body that are seldom exposed to
sunlight (Arch Environ Health 1990;45:261–267). Sun exposure is
associated with increased survival from melanoma (J Natl Cancer Inst
2005;97:195–199). Another study showed that people who had longer
lifetime exposure to the sun without burning were less likely to get
melanomas than those with less exposure (J Invest Dermatol
2003;120:1087–1093.)
The rise in skin cancers over the last 25 years parallels the rise
in use of sunscreen lotions, which block Vitamin D-producing UVB
radiation but not cancer-causing ultraviolet A radiation (UVA).
(Newer sunscreen lotions also block out UVA.)
The U.S. government and its citizens currently spend $2 trillion on
"health care," i.e., sickness care, each year. The cost of taking a
5,000 IU supplement of Vitamin D every day for a year is $22.00. The
cost for 300 million Americans taking this supplement would be $6.6
billion dollars. The number and variety of diseases that Vitamin D
at this dose could prevent, starting with a 50 percent reduction in
cancer, is mind-boggling. If everyone took 5,000 IU/day of Vitamin
D, the U.S. "health care" industry would shrink. It would no longer
account for 16 percent of the gross domestic product.
Source of information: Donald Miller is a cardiac surgeon and
Professor of Surgery at the University of Washington in Seattle. He
is a member of Doctors for Disaster Preparedness and writes articles
on a variety of subjects for LewRockwell.com. His web site is
www.donaldmiller.com
Article Link to actual article:
view link
Other Links:
Forbes.com September 10, 2007
Archives of Internal Medicine September 10, 2007;167:1730-1737
Lack of Sunshine Causes One Million Deaths a Year
Which Vitamin Will Improve Your Life Expectancy the Most?
Vitamin D Council - Dr.
John Cannell
Cancer Society's Anti‑Sun Ads Decried as Deceptive
Cancer Society’s Anti-Sun Ads Decried as Deceptive
Studies point to omega-6 / omega-3 imbalance as a
greater factor in skin cancer deaths;
Excessive sun avoidance may
raise overall cancer risk
There is no longer significant doubt that moderate sun exposure –
short of suffering frequent, substantial sunburns –actually reduces
cancer risk overall.
In fact, the reverse seems to be the case, as we report in elsewhere
in this issue. New research affirms prior indications that many
Americans – especially darker skinned people – lack sufficient
Vitamin D-generating (hence cancer-curbing) sun exposure.
The hypothesis that moderate sun exposure curbs cancer risks rests
on abundant evidence that Vitamin D probably ranks among the most
powerful anti-cancer factors in the human body.
A summer-season ad campaign from the American Cancer Society defies
the growing consensus concerning the causes of fatal skin cancers.
Sunscreen is certainly useful for preventing sunburn, which may be
responsible for a small percentage of the relatively small number of
fatal skin cancers that occur annually in the US.
Only fair-skinned people seem to run a substantial risk of
developing skin cancer in response to the kind of daylong sun
exposure hunting, gathering, and farming humans experienced
throughout millennia of evolution, until very recently.
But it is not clear that sun exposure is a huge risk even for them,
and there's much less that sun is a major risk factor among non-fair
folks.
The latest outrage against reason comes in the form of an
advertising campaign from the American Cancer Society (ACS) that’s
sponsored … silently … by Neutrogena: a major sunscreen maker.
This regrettable venture – whose anti-sun, pro-sunscreen message is
intended, ostensibly, to reduce the risk of fatal skin cancers –
could actually increase its largely female targets’ overall cancer
risk.
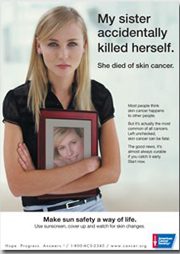
Under a headline that reads ““My sister accidentally killed herself.
She died of skin cancer”, the American Cancer Society’s new public
service ad shows a young woman holding up a photograph of a smiling
blonde.
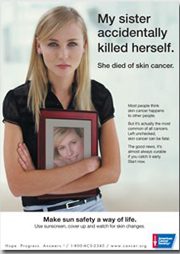 |
Appearing this summer in
more than a dozen women’s magazines, the ad says that
“left unchecked, skin cancer can be fatal,” and urges
its female targets to “use sunscreen, cover up and watch
for skin changes.”
Medical reporters at many major media outlets
interviewed leading skin cancer researchers, who
disputed the misleading message being foisted on
millions of women by the Cancer Society’s ads.
Ads paid by sunscreen maker distort reality Key
Points
Experts call Cancer Society’s pro-sunscreen ads
unscientific and unrealistic.Excessive sun avoidance could raise overall cancer
death rates, due to resulting drop in Vitamin D
production in people’s skin.Americans’ common omega-3/omega-6 intake imbalance may
be a much greater risk factor in skin cancer. |
|
But as The New York Times said about the ad, “The
woman in the picture is a model, not a skin cancer victim. And the
advertisement’s implicit message — that those who die of skin cancer
have themselves to blame — has provoked a sharp response from some
public-health doctors, who say the evidence simply does not
support it.”
The two key points made by experts interviewed by The New York
Times, ABC News, and others were these:
 | While most cases of skin cancer (carcinomas) may be caused by sun
overexposure, almost all of these cancers are innocuous and not
life-threatening. |
 | Even obsessive use of sunscreen may not prevent the most dangerous
kind of skin cancers, called melanomas.
In truth, by reducing blood levels of
Vitamin D, constant use of
sunscreen outdoors could raise the risk of many common, dangerous
malignancies, including ovarian, breast, kidney, and colon cancers.
(Not to mention the possible cancer causing substances that are
absorbed by the skin from the sun screens.) |
These are the basic facts, gleaned from the American Cancer Society,
the National Cancer Institute (NCI), the National Institutes of
Health (NIH), the World Health Organization (WHO), and leading
academic researchers:
Skin cancer is responsible for less than two percent of all cancer
deaths, accounting for about 11,000 of the 565,000 American cancer
deaths recorded in 2006.
Nearly all skin cancer deaths stem from relatively rare malignant
melanomas, which constitute only six percent of all skin-cancer
cases.
Sunscreen does not appear to prevent melanomas – the rarest but
most lethal skin cancers by far – in which genetic and nutritional
factors appear to play greater roles than sun exposure. Evidence for
a cause-and-effect link between excessive sun exposure and deadly
melanomas is weak.
Among melanoma cancer patients, those who reported more sun
exposure prior to their diagnosis enjoy higher survival rates,
compared with patients who reported less prior sun exposure.
(Schwartz GG, Skinner HG 2007)
Only one in five melanomas is estimated to be related to sun
exposure. This estimate comes from Howard L. Kaufman, M.D.,
co-director of the Melanoma Center at Columbia University.
How can the glaring discrepancies in experts’ estimates of the sun’s
proportionate role in causing melanomas, which range from 20 percent
up to 50 or 90 percent be explained? One possibility is that even if
UV sunrays do not generally cause melanomas, heavier sun exposure
among people with fair skin and those living in sunny climates could
promote growth of melanomas initiated by other causes, thereby
raising melanoma death rates in these groups.
We should stress that most deaths caused by generally non-fatal
carcinoma-type tumors (only 20 percent of all skin cancer
fatalities) appear linked to excessive sun exposure.
This is why research indicates that sunscreen can reduce the risk of
this least-dangerous category of skin cancers.
But one must weigh the best sunscreens’ ability to reduce the
already minuscule risk of death from skin carcinomas against three
countervailing factors:
The potential for increasing one’s risk of non-skin cancers, due to
reduced Vitamin D production.
 | The unknown risks of the insufficiently safety-tested additives in
sunscreens  | The substantial expense and hassle of doing what most
dermatologists advise, which is to apply hefty amounts of sunscreen
whenever one spends more than 20 minutes in the sun. | |
Dermatologists’ advice regarding sunscreen use and sun avoidance
makes the most sense for fair-skinned folks, who lack UV-blocking
pigment (melanin) in their skin, who can make extra efforts to get
ample dietary Vitamin D.
(Note: the most useful form of
Vitamin D is the D3 form found in
animal foods like fish, not the D2 form found in most Vitamin D and
multivitamin supplements.)
Given Americans’ increasingly indoor-oriented, sun-deprived lives,
most don’t consume enough Vitamin D from foods or supplements. This
is why most Vitamin D researchers want to raise the US recommended
daily allowance (RDA) from 400 IU to 1,000 or 2,000 IU, and urge
people to eat fatty fish (the best food source) and take higher
supplemental doses.
There is compelling evidence concerning the role of America’s
all-too-common omega-6/omega-3 fatty acid intake imbalance in
creating increased risk of skin cancers.
Researchers at the American Health Foundation (AHF) in Valhalla, New
York reported the results of a study using human skin cancer cells.
The AHF scientists introduced their findings by noting the growing
consensus that prompted their revealing test tube research:
“Epidemiological, experimental, and mechanistic data implicate omega-6 polyunsaturated fatty acids (PUFAs) as stimulators and
long-chain omega-3 PUFAs as inhibitors of … a range of human
cancers, including melanoma.” (Albino AP et al 200)
Omega-6 fatty acids predominate in America’s most common vegetable
oils (corn, soy, canola, safflower, sunflower, cottonseed) – thus in
most packaged and prepared foods – and in grain fed meats and
poultry.
Long-chain omega-3s – the most beneficial kind – are abundant only
in fish and fish oils, while the valuable but less beneficial
short-chain kind is abundant only in leafy green vegetables and
flaxseed or flaxseed oil.
Source of information: Vitaminal Choices, Craig Weatherby
view link
You should read the rest of this article.
This is a summary at best of the full article. |